In Ontario, Lyme disease is transmitted by an infected blacklegged (Ixodes scapularis) tick.
Blacklegged ticks are present in Simcoe and Muskoka, and locally acquired blacklegged ticks have tested positive for the bacteria that causes Lyme disease.
Ticks cannot jump or fly. When a person or animal brushes by vegetation, such as grass or shrubs along a forest trail that the tick is resting on, the tick climbs onto the person or animal in search of a place to bite and feed (exposed skin).
Just like mosquitoes, ticks survive on blood. They insert their mouthpart into the skin of a person or an animal to feed. An infected tick can spread the bacteria that causes Lyme disease to humans when they feed; however, if a tick is attached to your skin for less than 24 hours, your chance of getting Lyme disease is extremely low. Ticks are small and bites are usually painless which means without checking, you might not know that you have been bitten. It is important to check for and remove ticks as soon as possible to prevent Lyme disease.
What do blacklegged ticks look like?
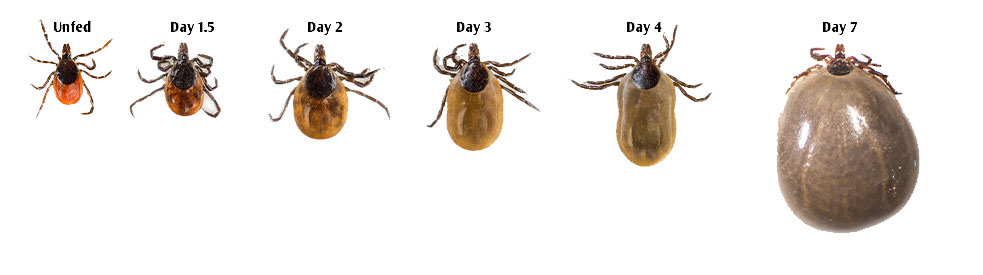
Blacklegged ticks are small. They range in size from a poppy seed to a pea (1-5 mm). A tick's size depends on its life stage (larva, nymph, adult), whether it has fed recently, and how long it has fed. If a tick has been attached to the skin for a few days, it can swell and appear brown or grey. If a swollen tick is on your skin, it may appear as a new skin tag or pimple.
The images below show how a blacklegged tick nymph (Figure 1) and adult-female (Figure 2) appear the longer they feed.
Figure 1: Nymph-Stage: Blacklegged Tick Growth
Image Source: URI TickEncounter Resource Center
Figure 2: Female Adult-Stage: Blacklegged Tick Growth
Image Source: URI TickEncounter Resource Center
Where are blacklegged ticks found?
The risk of being exposed to a blacklegged tick is highest in forests, wooded areas, and places with shrubs/bushes, tall grass, and leaf litter. Trails surrounded by mixed vegetation and the edges of these areas are also common areas where blacklegged ticks have been found. If you work outdoors or participate in outdoor activities (e.g., hiking, biking, fishing, camping, hunting, and golfing), you may be at risk of a tick bite. Ticks are most active in the spring, summer, and fall.
In Ontario, a map of blacklegged tick established risk areas is updated each year. This map identifies areas in Ontario where blacklegged ticks have been consistently found based on tick dragging (active surveillance). It is important to recognize that although this map identifies known risk areas, there is a chance of being exposed to an infected blacklegged tick anywhere in Ontario.